
Physiology
Basic Cellular
What is the approximate lifespan of the platelet:
Answer:
The normal platelet lifespan is 10 days.Platelets
Physiology / Basic Cellular / Blood and Blood Flow
Last Updated: 11th April 2022
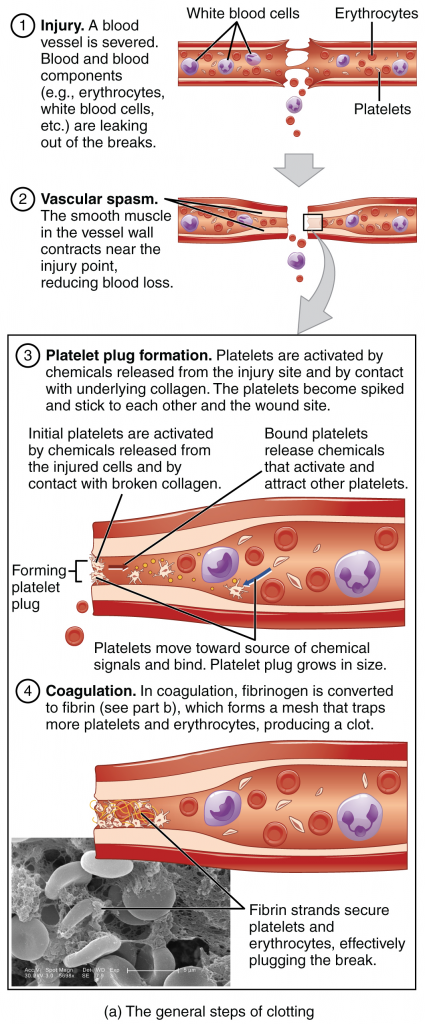
The normal haemostatic response to vascular damage depends on a closely linked interaction between the blood vessel wall, circulating platelets and blood coagulation factors.
Platelet Production
Platelets are produced in the bone marrow by fragmentation of the cytoplasm of megakaryocytes, derived from the common myeloid progenitor cell. The time interval from differentiation of the human stem cell to the production of platelets averages 10 days.
Thrombopoietin is the major regulator of platelet formation and 95% of this is produced by the liver.
The normal platelet count is approximately 150 - 450 x 109/L and the normal platelet lifespan is 10 days. Under normal circumstances, about one-third of the marrow output of platelets may be trapped at any one time in the normal spleen.

Platelet Production. (Image by パタゴニア [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)])
Platelet Structure
Platelets are extremely small and discoid. The platelet surface coat has glycoproteins that are particularly important in platelet adhesion and aggregation. Adhesion to collagen is facilitated by glycoprotein Ia. Glycoproteins Ib and IIb/IIIa are important in the attachment of platelets to von Willebrand factor (VWF) and hence to vascular subendothelium. The binding site for IIb/IIIa is also the receptor for fibrinogen, which, like VWF, is important in platelet-platelet aggregation.
The platelet plasma membrane invaginates into the platelet interior to form a canalicular system which provides a large reactive surface area to which the plasma coagulation proteins may be selectively absorbed. Plasma membrane phospholipids are particularly important in the conversion of factor X to Xa and prothrombin (factor II) to thrombin (IIa).
Platelets contain three types of storage granule;
- dense granules containing ADP, ATP, serotonin and calcium
- alpha granules containing clotting factors, von Willebrand factor (VWF), platelet-derived growth factor (PDGF) and other proteins
- lysosomes containing hydrolytic enzymes
Platelets are also rich in signalling and cytoskeletal proteins, which support the rapid switch from quiescence to activation that follows vessel damage. During the release reaction, the contents of the granules are discharged into the open canalicular system.
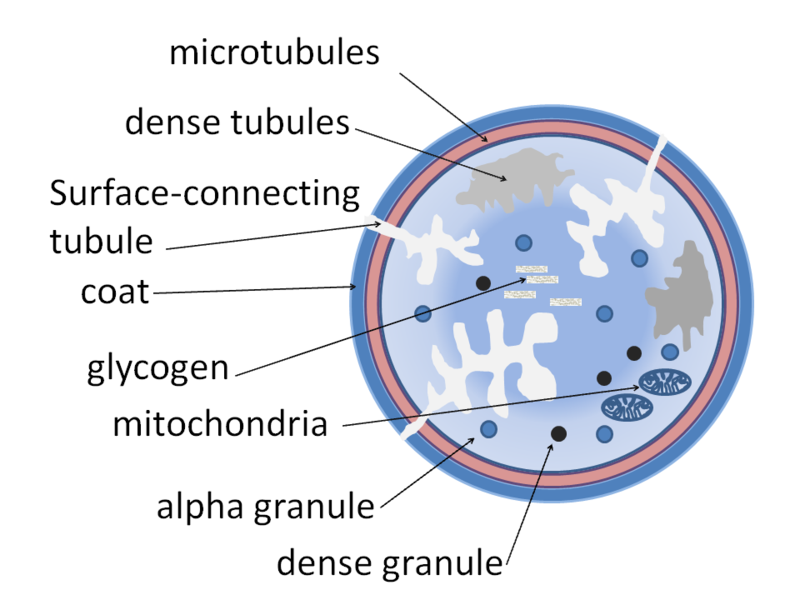
Platelet Structure. (Image by Dr Graham Beards [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)])
Platelet Function
The primary function of platelets is the formation of a platelet plug during the primary haemostatic response to vascular injury via adhesion, aggregation and activation. The immobilisation of platelets at the sites of vascular injury requires specific platelet-vessel wall (adhesion) and platelet-platelet (aggregation) reactions, both partly mediated through VWF. Platelet aggregation is characterised by cross-linking of platelets through active GPIIb/IIIa receptors with fibrinogen bridges.
Primary activation by various agonists (e.g. thrombin) induces intracellular signalling, leading to the release of alpha granule contents. These have an important role in platelet aggregate formation and stabilisation and, in addition, the ADP released from dense granules has a major positive feedback role in promoting platelet activation.
Thromboxane A2 (TXA2), produced by platelets, is important in secondary amplification of platelet activation to form a stable platelet aggregate. TXA2 lowers platelet cAMP levels and initiates the platelet release reaction; it also has powerful vasoconstrictive activity.
After platelet aggregation and release, the exposed membrane phospholipid is available for two reactions in the coagulation cascade. The first involves factors IXa, VIIIa and X in the formation of factor Xa. The second results in the formation of thrombin from the interactions of factors Xa, Va and prothrombin.
PDGF found in the alpha granules of platelets stimulates vascular smooth muscle cells to multiply and thus may hasten vascular healing following injury.
Primary Haemostasis. (Image by OpenStax College [CC BY 3.0 (https://creativecommons.org/licenses/by/3.0)])
Natural Inhibitors of Platelet Function
The release reaction is inhibited by substances that increase the level of platelet cAMP. Prostacyclin (PGI2), synthesised by endothelial cells, is one such substance. PGI2 has the opposing effects of TXA2; it is a potent inhibitor of platelet adhesion and aggregation on normal vascular endothelium (and a potent vasodilator). Nitric oxide is constitutively released from endothelial cells and also from macrophages and platelets; it inhibits platelet activation and promotes vasodilation.
Report A Problem
Is there something wrong with this question? Let us know and we’ll fix it as soon as possible.
Loading Form...
- Biochemistry
- Blood Gases
- Haematology
| Biochemistry | Normal Value |
|---|---|
| Sodium | 135 – 145 mmol/l |
| Potassium | 3.0 – 4.5 mmol/l |
| Urea | 2.5 – 7.5 mmol/l |
| Glucose | 3.5 – 5.0 mmol/l |
| Creatinine | 35 – 135 μmol/l |
| Alanine Aminotransferase (ALT) | 5 – 35 U/l |
| Gamma-glutamyl Transferase (GGT) | < 65 U/l |
| Alkaline Phosphatase (ALP) | 30 – 135 U/l |
| Aspartate Aminotransferase (AST) | < 40 U/l |
| Total Protein | 60 – 80 g/l |
| Albumin | 35 – 50 g/l |
| Globulin | 2.4 – 3.5 g/dl |
| Amylase | < 70 U/l |
| Total Bilirubin | 3 – 17 μmol/l |
| Calcium | 2.1 – 2.5 mmol/l |
| Chloride | 95 – 105 mmol/l |
| Phosphate | 0.8 – 1.4 mmol/l |
| Haematology | Normal Value |
|---|---|
| Haemoglobin | 11.5 – 16.6 g/dl |
| White Blood Cells | 4.0 – 11.0 x 109/l |
| Platelets | 150 – 450 x 109/l |
| MCV | 80 – 96 fl |
| MCHC | 32 – 36 g/dl |
| Neutrophils | 2.0 – 7.5 x 109/l |
| Lymphocytes | 1.5 – 4.0 x 109/l |
| Monocytes | 0.3 – 1.0 x 109/l |
| Eosinophils | 0.1 – 0.5 x 109/l |
| Basophils | < 0.2 x 109/l |
| Reticulocytes | < 2% |
| Haematocrit | 0.35 – 0.49 |
| Red Cell Distribution Width | 11 – 15% |
| Blood Gases | Normal Value |
|---|---|
| pH | 7.35 – 7.45 |
| pO2 | 11 – 14 kPa |
| pCO2 | 4.5 – 6.0 kPa |
| Base Excess | -2 – +2 mmol/l |
| Bicarbonate | 24 – 30 mmol/l |
| Lactate | < 2 mmol/l |

