
Pathology
Immune Responses
Regarding monocytes, which of the following statements is CORRECT:
Answer:
Monocytes account for 5 - 10% of the peripheral white cell count. Monocytes are usually larger than other peripheral blood leucocytes and have a large central oval or indented nucleus with clumped chromatin. The abundant cytoplasm stains blue and contains many fine vacuoles, giving a ground-glass appearance. Cytoplasmic granules are also often present. Monocytes divide and differentiate from the granulocyte macrophage progenitor into monoblasts, promonocytes, monocytes and tissue macrophages (in increasing order of maturity). Monocytes spend only a short time in the marrow and, after circulating for 20-40 hours, leave the blood to enter the tissues where they become macrophages.Phagocytes
Pathology / Immune Responses
Last Updated: 6th December 2020
Phagocytes can be divided into granulocytes (neutrophils, eosinophils and basophils) and monocytes.
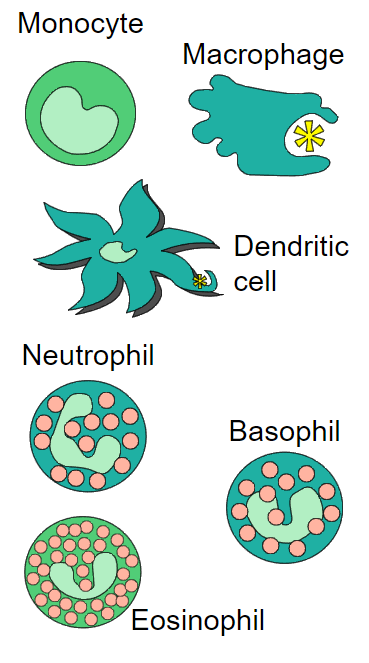
Phagocytes. (Image by Unknown. [Public domain])
Granulopoiesis
Granulocytes and monocytes are formed in the bone marrow from a common precursor cell. The earliest recognisable granulocyte precursors are myeloblasts, which undergo further differentiation into promyelocytes, myelocytes, metamyelocytes and finally, mature granulocytes. The bone marrow normally contains more myeloid cells than erythroid cells in the ratio of 2:1 to 12:1, the largest proportion being neutrophils and metamyelocytes.
Many growth factors are involved in this process; they stimulate proliferation and differentiation and affect the function of the mature cells on which they act. They also inhibit apoptosis. Increased granulocyte (and monocyte) production in response to an infection is induced by increased production of growth factors from stromal cells and T lymphocytes, stimulated by endotoxin and cytokines such as IL-1 or tumour necrosis factor (TNF).
Following their release from the marrow, granulocytes spend only 6-10 hours in the circulation before entering tissues where they perform their phagocytic function. They spend on average 4-5 days in the tissues before they are destroyed during defensive action or as the result of senescence. In the bloodstream there are two pools usually of about equal size: the circulating pool (included in the blood count) and the marginating pool (not included in the blood count).
Neutrophils
Neutrophils are the most abundant peripheral blood leucocyte, comprising about 50 - 70% of circulating white cells. Neutrophils have a characteristic dense nucleus consisting of between two and five lobes, and a pale cytoplasm with an irregular outline containing many fine pink-blue or grey-blue granules. The granules are divided into primary, which appear at the promyelocyte stage, and secondary, which appear at the myelocyte stage and predominate in the mature nucleus. Both types of granule are lysosomal in origin; the primary contains myeloperoxidase and other acid hydrolases; the secondary contains lactoferrin, lysozyme and other enzymes. The lifespan of neutrophils in the blood is only 6 – 10 hours. In response to tissue damage, cytokines and complement proteins, neutrophils migrate from the bloodstream to the site of insult within minutes, where they destroy pathogens by phagocytosis.
Eosinophils
Eosinophils comprise 1 - 3% of circulating white cells. Eosinophils are similar to neutrophils, except that the cytoplasmic granules are coarser and more deeply red staining, and there are rarely more than three nuclear lobes. They are less motile, but longer lived. They enter inflammatory exudates and have a special role in allergic responses, defence against parasites and removal of fibrin formed during inflammation. Thus they play a role in local immunity and tissue repair.
Basophils and Mast Cells
Basophils are only occasionally seen in normal peripheral blood comprising < 1% of circulating white cells. However, they are the largest type of granulocyte. They have many dark cytoplasmic granules which overlie the nucleus and contain heparin and histamine. They have immunoglobulin E (IgE) attachment sites and their degranulation is associated with histamine release. Basophils are very similar in both appearance and function to mast cells.
Mast cells are resident in tissues and have an important function in allergy, anaphylaxis and defence against parasites. Mast cells have granules containing preformed mediators such as tryptase, histamine, serotonin and heparin and can also secrete newly formed mediators such as prostaglandin D2, bradykinin, cytokines and leukotrienes. Mast cell degranulation is triggered by cross-linking of high affinity receptors for the Fc portion of IgE and results in: increased capillary permeability, vasodilation, smooth muscle contraction, platelet aggregation and activation, complement activation, increased mucus secretion and chemotaxis of leucocytes.
Monocytes and Macrophages
Monocytes account for 5 - 10% of the peripheral white cell count. Monocytes are usually larger than other peripheral blood leucocytes and have a large central oval or indented nucleus with clumped chromatin. The abundant cytoplasm stains blue and contains many fine vacuoles, giving a ground-glass appearance. Cytoplasmic granules are also often present. Monocytes divide and differentiate from the granulocyte macrophage progenitor into monoblasts, promonocytes, monocytes and tissue macrophages (in increasing order of maturity). Monocytes spend only a short time in the marrow and, after circulating for 20-40 hours, leave the blood to enter the tissues where they become macrophages.
Macrophages form the reticuloendothelial system in the liver, spleen and lymph nodes. The lifespan of macrophages may be as long as several months or even years. In tissues the macrophages become self-replicating without replenishment from the blood. They assume specific functions in different tissues e.g. Kupffer cells in the liver, alveolar macrophages in the lung, intraglomerular mesangial cells in the kidneys, microglial cells in the brain, Langerhans cells in the skin and histiocytes in connective tissue. Macrophages may be activated by cytokines such as IFN-gamma, contact with complement or direct contact with the target cell through leucocyte adhesion molecules.
Normal Function
Neutrophils, eosinophils, basophils and monocytes all have phagocytic activity, but neutrophils and monocytes are the main professional phagocytes. The normal function of neutrophils and monocytes may be divided into three phases:
- Chemotaxis (cell mobilisation and migration):
- The phagocyte is attracted to bacteria or the site of inflammation by chemotactic substances released from damaged tissues, by complement components and by the interaction of leucocyte adhesion molecules with ligands on the damaged tissues. The leucocyte adhesion molecules also mediate recruitment and interaction with other immune cells.
- Phagocytosis:
- The foreign material or dead/damaged host cells are phagocytosed. Recognition of a foreign particle is aided by opsonisation with immunoglobulin or complement because both neutrophils and monocytes have Fc and C3b receptors. Macrophages have a central role in antigen presentation: processing and presenting foreign antigens on human leucocyte antigen (HLA) molecules to the immune system. They also secrete a large number of growth factors and chemokines which regulate inflammation and immune responses.
- Killing and Digestion:
- This occurs by oxygen-dependent and oxygen-independent pathways.
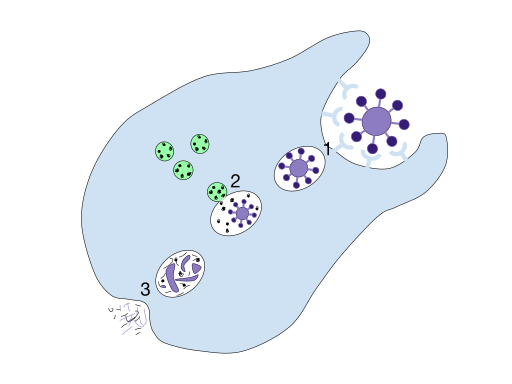
Process of phagocytosis: 1. A particle is ingested by a phagocyte after antigens are recognized which results in the formation of a phagosome. 2. The fusion of lysosomes with the phagosome creates a phagolysosome. The particle is broken down by the digestive enzymes found in the lysosomes. 3. The resulting waste material is discharged from the phagocyte by exocytosis. (Image by Mango Slices [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)])
Report A Problem
Is there something wrong with this question? Let us know and we’ll fix it as soon as possible.
Loading Form...
- Biochemistry
- Blood Gases
- Haematology
| Biochemistry | Normal Value |
|---|---|
| Sodium | 135 – 145 mmol/l |
| Potassium | 3.0 – 4.5 mmol/l |
| Urea | 2.5 – 7.5 mmol/l |
| Glucose | 3.5 – 5.0 mmol/l |
| Creatinine | 35 – 135 μmol/l |
| Alanine Aminotransferase (ALT) | 5 – 35 U/l |
| Gamma-glutamyl Transferase (GGT) | < 65 U/l |
| Alkaline Phosphatase (ALP) | 30 – 135 U/l |
| Aspartate Aminotransferase (AST) | < 40 U/l |
| Total Protein | 60 – 80 g/l |
| Albumin | 35 – 50 g/l |
| Globulin | 2.4 – 3.5 g/dl |
| Amylase | < 70 U/l |
| Total Bilirubin | 3 – 17 μmol/l |
| Calcium | 2.1 – 2.5 mmol/l |
| Chloride | 95 – 105 mmol/l |
| Phosphate | 0.8 – 1.4 mmol/l |
| Haematology | Normal Value |
|---|---|
| Haemoglobin | 11.5 – 16.6 g/dl |
| White Blood Cells | 4.0 – 11.0 x 109/l |
| Platelets | 150 – 450 x 109/l |
| MCV | 80 – 96 fl |
| MCHC | 32 – 36 g/dl |
| Neutrophils | 2.0 – 7.5 x 109/l |
| Lymphocytes | 1.5 – 4.0 x 109/l |
| Monocytes | 0.3 – 1.0 x 109/l |
| Eosinophils | 0.1 – 0.5 x 109/l |
| Basophils | < 0.2 x 109/l |
| Reticulocytes | < 2% |
| Haematocrit | 0.35 – 0.49 |
| Red Cell Distribution Width | 11 – 15% |
| Blood Gases | Normal Value |
|---|---|
| pH | 7.35 – 7.45 |
| pO2 | 11 – 14 kPa |
| pCO2 | 4.5 – 6.0 kPa |
| Base Excess | -2 – +2 mmol/l |
| Bicarbonate | 24 – 30 mmol/l |
| Lactate | < 2 mmol/l |

