
Physiology
Renal
In which part of the loop of Henle is Na+ reabsorbed via the Na+/K+/2Cl- symporter:
Answer:
In the thick ascending limb, Na+ and Cl- ions are actively reabsorbed from the tubular fluid via the Na+/K+/2Cl- symporter on the apical membrane. The Na+ ions are primarily transported across the basolateral membrane by Na+ pumps and the Cl- ions by diffusion. K+ leaks back into the tubular fluid via apical ROMK K+ channels creating a positive charge that drives the reabsorption of cations (Na+, K+, Ca2+, Mg2+) through paracellular pathways. As the thick ascending limb is impermeable to water, the reabsorption of ions reduces the tubular fluid osmolality, and increases the interstitial fluid osmolality, creating an osmotic difference.Loop of Henle
Physiology / Renal / Mechanism of Filtration
Last Updated: 26th July 2024
The loop of Henle consists of a single layer of flattened squamous cells (transitioning to columnar cells in the thick ascending segment), which form a thin-walled hairpin-shaped tube. At the point at which the loop associates with the juxtaglomerular apparatus after re-entering the cortex, the wall is formed from modified macula densa cells.
About 25% of filtered Na+ and Cl-, and 15% of filtered water and cations such as K+, Ca2+, Mg2+ are reabsorbed in the loop of Henle.
The generation of high osmolality in the medulla depends on the differential permeabilities to water and solutes in different regions, the active transport of ions in the thick ascending limb and the countercurrent multiplier. Tubular fluid is isotonic with plasma when it enters the loop of Henle, hypertonic at the tip of the hairpin (where it reaches equilibrium with the hypertonic interstitial fluid), and hypotonic when it leaves to enter the distal nephron.
Differential Permeabilities to Water and Solutes in Different Regions
- The thin descending limb of the loop of Henle is permeable to water and impermeable to NaCl and urea.
- The thin ascending limb is impermeable to water, but highly permeable to urea and NaCl.
- The thick ascending limb is impermeable to water and actively reabsorbs NaCl from tubular fluid.

Permeabilities of the Loop of Henle. (Image by OpenStax College [CC BY 3.0 , via Wikimedia Commons)
Active Transport of Ions in the Thick Ascending Limb
In the thick ascending limb, Na+ and Cl- ions are actively reabsorbed from the tubular fluid via the Na+/K+/2Cl- symporter on the apical membrane. The Na+ ions are primarily transported across the basolateral membrane by Na+ pumps and the Cl- ions by diffusion. K+ leaks back into the tubular fluid via apical ROMK K+ channels creating a positive charge that drives the reabsorption of cations (Na+, K+, Ca2+, Mg2+) through paracellular pathways. As the thick ascending limb is impermeable to water, the reabsorption of ions reduces the tubular fluid osmolality, and increases the interstitial fluid osmolality, creating an osmotic difference.
Countercurrent Multiplier
This increased interstitial fluid osmolality causes water to move passively out of the thin descending limb, concentrating the tubular fluid. As this concentrated fluid descends, it travels in the opposite direction to fluid returning from the still higher osmolality regions of the deep medulla. This countercurrent arrangement creates an osmotic gradient, causing Na+ and Cl- to diffuse out of the ascending limb (diluting the ascending fluid) and water to diffuse out of the descending limb (further concentrating the descending fluid). This effect is potentiated by the fact that the ascending limb is impermeable to water but highly permeable to Na+ and Cl-, and also by the recycling of urea between the collecting ducts and ascending limb, which makes an important contribution to urine concentration. At the tip of the loop of Henle, the interstitial fluid reaches its highest osmolality due in equal parts to NaCl and urea.
The blood supply to the medulla is prevented from dissipating the osmotic gradient between the cortex and medulla by the countercurrent exchanger arrangement of the vasa recta capillaries. The vasa recta also removes water reabsorbed from the loop of Henle and medullary collecting ducts.
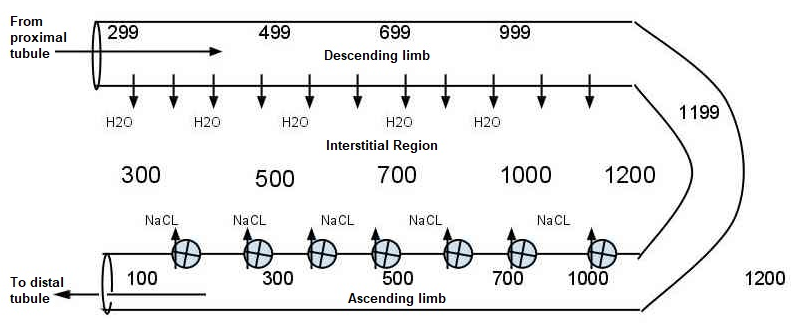
Countercurrent Multiplier. (Image by Pashute (Own work) [CC0], via Wikimedia Commons)
Report A Problem
Is there something wrong with this question? Let us know and we’ll fix it as soon as possible.
Loading Form...
- Biochemistry
- Blood Gases
- Haematology
| Biochemistry | Normal Value |
|---|---|
| Sodium | 135 – 145 mmol/l |
| Potassium | 3.0 – 4.5 mmol/l |
| Urea | 2.5 – 7.5 mmol/l |
| Glucose | 3.5 – 5.0 mmol/l |
| Creatinine | 35 – 135 μmol/l |
| Alanine Aminotransferase (ALT) | 5 – 35 U/l |
| Gamma-glutamyl Transferase (GGT) | < 65 U/l |
| Alkaline Phosphatase (ALP) | 30 – 135 U/l |
| Aspartate Aminotransferase (AST) | < 40 U/l |
| Total Protein | 60 – 80 g/l |
| Albumin | 35 – 50 g/l |
| Globulin | 2.4 – 3.5 g/dl |
| Amylase | < 70 U/l |
| Total Bilirubin | 3 – 17 μmol/l |
| Calcium | 2.1 – 2.5 mmol/l |
| Chloride | 95 – 105 mmol/l |
| Phosphate | 0.8 – 1.4 mmol/l |
| Haematology | Normal Value |
|---|---|
| Haemoglobin | 11.5 – 16.6 g/dl |
| White Blood Cells | 4.0 – 11.0 x 109/l |
| Platelets | 150 – 450 x 109/l |
| MCV | 80 – 96 fl |
| MCHC | 32 – 36 g/dl |
| Neutrophils | 2.0 – 7.5 x 109/l |
| Lymphocytes | 1.5 – 4.0 x 109/l |
| Monocytes | 0.3 – 1.0 x 109/l |
| Eosinophils | 0.1 – 0.5 x 109/l |
| Basophils | < 0.2 x 109/l |
| Reticulocytes | < 2% |
| Haematocrit | 0.35 – 0.49 |
| Red Cell Distribution Width | 11 – 15% |
| Blood Gases | Normal Value |
|---|---|
| pH | 7.35 – 7.45 |
| pO2 | 11 – 14 kPa |
| pCO2 | 4.5 – 6.0 kPa |
| Base Excess | -2 – +2 mmol/l |
| Bicarbonate | 24 – 30 mmol/l |
| Lactate | < 2 mmol/l |

