
Anatomy
Head and Neck
The anaesthetist is attempting to intubate an unconscious patient who is unable to maintain their airway. The anaesthetist finds himself in a 'can't intubate, can't ventilate' situation and proceeds to perform an emergency tracheotomy. Which of the following structures are most likely damaged in this procedure:
Answer:
Structures particularly vulnerable in tracheostomy include the isthmus of the thyroid, the jugular arch connecting the anterior jugular veins, the inferior thyroid vein, the left brachiocephalic vein, the thyroidea ima artery, and the recurrent laryngeal nerve (less commonly).Trachea (Neck)
Anatomy / Head and Neck / Neck
Last Updated: 11th April 2019
The trachea begins at vertebral level C6, where it is continuous with the larynx above. The trachea lies directly anterior to the oesophagus and travels inferiorly to pass through the thoracic inlet.
Cricothyrotomy
A cricothyrotomy is performed to provide a temporary emergency airway in situations where there is obstruction at or above the level of the larynx, such that oral/nasal endotracheal intubation is impossible e.g. as a result of inhalation of a foreign body, severe oedema secondary to anaphylactic reaction, or severe head and neck trauma.
Compared with an emergency tracheostomy, it is quicker and easier to perform and associated with fewer complications. It involves making an opening in the median cricothyroid ligament (the medial part of the cricothyroid membrane), between the cricoid and thyroid cartilages of the larynx. The ligament can be palpated in the midline and usually there are only small blood vessels, connective tissue and skin overlying it.
![By Olek Remesz (wiki-pl: Orem, commons: Orem) [CC BY-SA 2.5-2.0-1.0], via Wikimedia Commons](https://mrcemsuccess.com/wp-content/uploads/2016/07/larynx-1024x887.png)
Structure of the Larynx (Anterior View). (Image by Olek Remesz (wiki-pl: Orem, commons: Orem) [CC BY-SA 2.5-2.0-1.0], via Wikimedia Commons)
Tracheostomy
At a lower level, the airway can be accessed surgically (or percutaneously) through the anterior wall of the trachea by tracheostomy. Tracheostomy is usually performed in non-emergency situations.
A small transverse incision is placed in the lower third of the neck anteriorly. The strap (infrahyoid) muscles are deviated laterally and the trachea can be easily visualised. Occasionally it is necessary to divide the isthmus of the thyroid. An incision is typically made between the second and third or the third and fourth tracheal rings and a small tracheostomy tube inserted.
This route of entry is complicated because large veins and part of the thyroid gland overlie this region. Structures particularly vulnerable include the isthmus of the thyroid, the jugular arch connecting the anterior jugular veins, the inferior thyroid vein, the left brachiocephalic vein, the thyroidea ima artery, and the recurrent laryngeal nerve (less commonly).
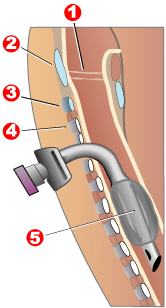
Completed Tracheostomy: 1) Vocal folds, 2) Thyroid cartilage, 3) Cricoid cartilage, 4) Tracheal rings, 5) Balloon cuff. (Image by Jeremykemp [Copyrighted free use], via Wikimedia Commons)
Report A Problem
Is there something wrong with this question? Let us know and we’ll fix it as soon as possible.
Loading Form...
- Biochemistry
- Blood Gases
- Haematology
| Biochemistry | Normal Value |
|---|---|
| Sodium | 135 – 145 mmol/l |
| Potassium | 3.0 – 4.5 mmol/l |
| Urea | 2.5 – 7.5 mmol/l |
| Glucose | 3.5 – 5.0 mmol/l |
| Creatinine | 35 – 135 μmol/l |
| Alanine Aminotransferase (ALT) | 5 – 35 U/l |
| Gamma-glutamyl Transferase (GGT) | < 65 U/l |
| Alkaline Phosphatase (ALP) | 30 – 135 U/l |
| Aspartate Aminotransferase (AST) | < 40 U/l |
| Total Protein | 60 – 80 g/l |
| Albumin | 35 – 50 g/l |
| Globulin | 2.4 – 3.5 g/dl |
| Amylase | < 70 U/l |
| Total Bilirubin | 3 – 17 μmol/l |
| Calcium | 2.1 – 2.5 mmol/l |
| Chloride | 95 – 105 mmol/l |
| Phosphate | 0.8 – 1.4 mmol/l |
| Haematology | Normal Value |
|---|---|
| Haemoglobin | 11.5 – 16.6 g/dl |
| White Blood Cells | 4.0 – 11.0 x 109/l |
| Platelets | 150 – 450 x 109/l |
| MCV | 80 – 96 fl |
| MCHC | 32 – 36 g/dl |
| Neutrophils | 2.0 – 7.5 x 109/l |
| Lymphocytes | 1.5 – 4.0 x 109/l |
| Monocytes | 0.3 – 1.0 x 109/l |
| Eosinophils | 0.1 – 0.5 x 109/l |
| Basophils | < 0.2 x 109/l |
| Reticulocytes | < 2% |
| Haematocrit | 0.35 – 0.49 |
| Red Cell Distribution Width | 11 – 15% |
| Blood Gases | Normal Value |
|---|---|
| pH | 7.35 – 7.45 |
| pO2 | 11 – 14 kPa |
| pCO2 | 4.5 – 6.0 kPa |
| Base Excess | -2 – +2 mmol/l |
| Bicarbonate | 24 – 30 mmol/l |
| Lactate | < 2 mmol/l |

