Revision Resources
Recent Posts View All
March FOAMed
Prostatitis
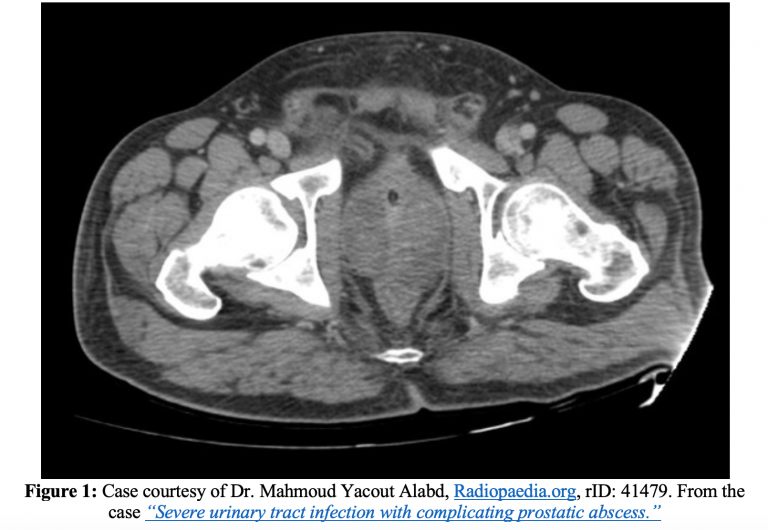
A 68-year-old male with a history of insulin-dependent diabetes mellitus, benign prostatic hypertrophy (BPH) and hypertension (HTN) presents to the ED with fatigue, subjective fevers for two days, and dysuria. He endorses myalgias and lower back discomfort. He denies any recent surgeries, procedures, or antibiotic use. He had an episode of non-bloody, non-bilious vomiting prior to arrival. The patient reports his blood sugars at home today were 273 and 315. He’s currently complaining of bladder pressure and has not voided in 6 hours. He is tachycardic and febrile.
Real world outcomes from TBI

Des Gorman talks about real-world outcomes and controversies following traumatic brain injury. His extensive research and experience in this area give a unique insight into what actually happens to the patients we care for.
Malaria

A 42-year-old male presents with headache, fever, chills, nausea, and myalgias. He denies cough, shortness of breath, vomiting, diarrhea, and neck stiffness, but states he returned from a month-long trip to Africa several weeks ago.
On examination, he is tachycardic and febrile. You do not find a rash or meningismus, but you palpate an enlarged spleen and liver.
What is your next step in evaluation and management?
Hypoglycaemia in Adults

In diabetics, hypoglycaemia is defined as a CBG <4.00 mmol/L (‘four is the floor’).
In non-diabetics, hypoglycaemia is often defined as a CBG <3.3 mmol/L.
Post Myocardial Infarction Complications – Stent Thrombosis

A 63-year-old male presents to the ED via EMS with chest pressure that he rates 10/10. He is sweating, uncomfortable, and states that this pain feels exactly like the heart attack he had 8 months ago. At that time, he was transferred to a PCI center, had a drug eluting stent placed, and has been compliant with his dual antiplatelet therapy. He tried some GTN at home, which did not help his pain.
As you move the patient over from the stretcher to the ED bed, EMS hands you the ECG that they obtained en route.
Are you sure you wish to end this session?

