Revision Resources
Recent Posts View All
March 2019 FOAMed
Ovarian Torsion
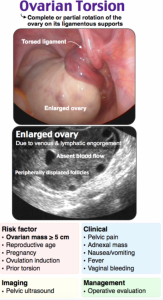
A 30-year-old female presents to the ED with right lower quadrant and flank pain that started 6 hours ago. The patient reports sudden onset pain that is progressively worsening, refractory to ibuprofen. She denies fevers, rigors, or dysuria, but endorses constant nausea and non-bloody, non-bilious emesis. Review of systems is unremarkable. Vital signs include BP 125/60, HR 107, T 100.2 oral, RR 15, SpO2 98% on room air.
Pertinent physical examination findings:
General: Alert and oriented x 3, though visibly uncomfortable
CV and lungs: Tachycardic, otherwise normal
Abdomen: Tender in RLQ, +rebounding, +guarding. No CVA tenderness // Pelvic: Significant tenderness along right adnexa
What’s the next step in your evaluation and treatment?
Management of Electrical Storm

The patient certainly looks uncomfortable as EMS roles him in. He is sweaty and anxious. As they roll down the EMS hallway, he gives a sharp scream of pain. “He’s been doing that for an hour doc. He has an ICD in place, and it is going off every 5 minutes or so. The monitor has been showing V Tach. The shocks seem to work about half the time, but only briefly. The ICD was placed because of a V tach arrest 2 years ago. He has a history of ischemic heart disease. His latest vitals are HR 186, BP 105/60, RR 24, and he is satting 93% on room air.” You pull the closet resident into the room. “Have you ever managed electrical storm?”
EM Boards Survival Guide: ENT 1

This week’s EM Board Survival Guide covers the must-knows for the inservice exam concerning ENT. This post also features stellar artwork from Dr. Katy Hanson at Hanson’s Anatomy.
Elbow Injuries – Ten Pitfalls in Diagnosis and Management
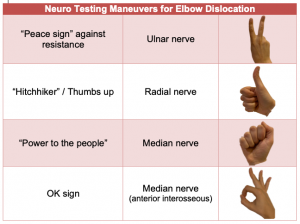
Although it doesn’t get the spotlight much in emergency medicine, the ED diagnosis and management of elbow injuries is of significant clinical importance. There are several easy-to-miss injuries that can lead to functional impairment. Even minor errors in management can result in long term consequences for patients. In this EM Cases main episode podcast with Dr. Arun Sayal, the brains behind the CASTED Course and Dr. Dale Dantzer, upper extremity orthopedic surgeon at North York General Hospital, we discuss pitfalls in the diagnosis and management of elbow injuries and answer questions such as: What is an easy way to remember the surgical indications for radial head fractures? What is the significance of a coronoid process fracture and how does it change management when seen with a radial head fracture? What is the best way to assess for pronation and supination of the forearm?
Nuances to the Management of Febrile Patients: Non-Infectious Causes of Fever

A 45-year-old woman presents to the emergency department with the chief complaint of “fever.” She has noted an intermittent fever for the last 2 weeks, with a maximum temperature of 103°F. She denies other symptoms. She was recently started on phenytoin for a newly-diagnosed seizure disorder, but she denies other medical history and she takes no other medications. Upon presentation, her vital signs are BP 118/72, HR 77, RR 14, SpO2 100%, T 102.2°F. Her exam is normal. Because this fever has been intermittent for several weeks, you think to yourself, “How should I approach this patient? Since her fever has lasted for 2 weeks without other symptoms, could there be a non-infectious cause? What pathologies cause non-infectious fever?”
Are you sure you wish to end this session?

