Revision Resources
Recent Posts View All
June FOAMed
Communicating Clearly

Communication is vital to all that we do – from the first contact with a patient, through history taking and examination, to initiating treatment and explaining procedures. We have to do our very best to get it right. This is perhaps even more important, and more difficult, in the pre-hospital field, where stress levels are high, the environment can be unpredictable and time is short. Clinicians meeting patients for the first time need to quickly assess the situation and also win trust and gain understanding.
Eclampsia in the ED

A 27-year-old P3G3 woman is found by her partner seizing at home one-week post-partum from a preterm (31 weeks + 4 days) pregnancy complicated by gestational hypertension. She was unable to schedule obstetric appointments during her second trimester due to loss of her insurance. She had been complaining of a headache earlier in the day, worsening prior to the seizure. On arrival to the patient’s home, paramedics find her altered, weak, and incontinent of urine. Pre-hospital vital signs included a heart rate of 110 bpm and a blood pressure of 180/110 mmHg. En route to the emergency department (ED), paramedics witnessed a second generalized seizure, started an IV, and administered midazolam. She continued to seize, requiring a repeat dose of midazolam. As she is transferred from the stretcher to a hospital bed, she has a third seizure with tonic/clonic activity.
Hypocalcaemia, Trauma and Major Transfusion
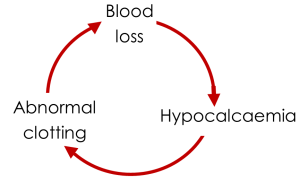
You are attending a road traffic collision as part of the pre hospital team and your patient is hypotensive and tachycardic with abdominal tenderness, especially in the left upper quadrant and obvious bleeding from an open fracture of the tibia and fibula. You have reduced the fracture, applied a pelvic binder, and given pain relief and tranexamic acid and have decided to commence a blood transfusion. You wonder if there is any benefit (or harm) in giving a bolus of calcium alongside the other therapies?
IUD Complications
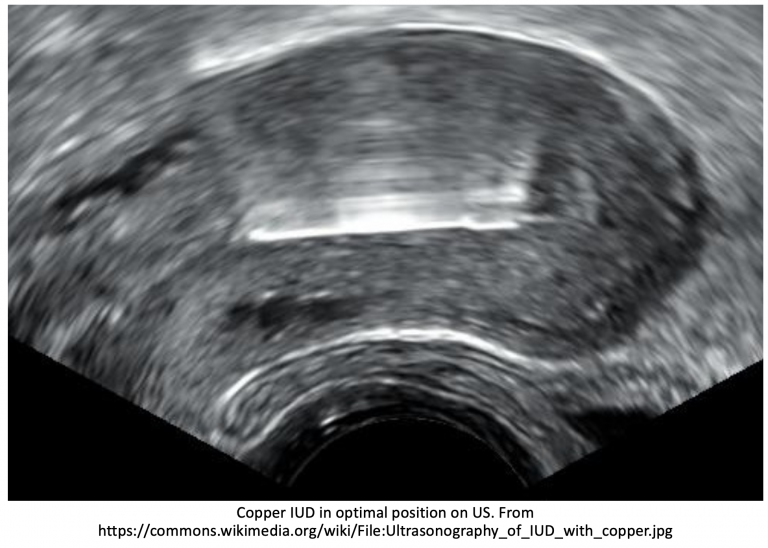
A 24-year-old female presents to the ED for pelvic pain that started 8 hours ago. The patient reports sudden onset pain this afternoon that is getting progressively worse, refractory to ibuprofen. She denies any fevers, rigors, or dysuria, but endorses constant pelvic pain, nausea, and vaginal bleeding. The patient has not had unprotected sex and no history of sexually transmitted infections.
Exam includes BP 115/68, HR 113, T 99.1 oral, RR 16, SpO2 98% on room air. She appears visibly uncomfortable, has dry mucous membranes, and is tender in the suprapubic area. Pelvic exam reveals scant blood per os, IUD strings seen, and she has pain with bimanual uterine palpation.
What’s the next step in your evaluation and treatment?
Are you sure you wish to end this session?

