Revision Resources
Recent Posts View All
February FOAMed
Decision Making in EM

Brit Long, MD (@long_brit) interviews Andrew Petrosoniak, MD, MSc, FRCPCP (@petrosoniak) on decision making in emergency medicine.
Andrew is a world-renowned leader in decision making and trauma. He is currently an EM attending physician, assistant professor at St. Michael’s Hospital, University of Toronto.
Push-Dose Epi

Push-dose epinephrine, or low-dose bolus epinephrine, can be given safely in adults and children. In children, consider for severe anaphylaxis or asthma resistant to IM administration, or for peri-intubation.
Acute Hemolytic Anemia
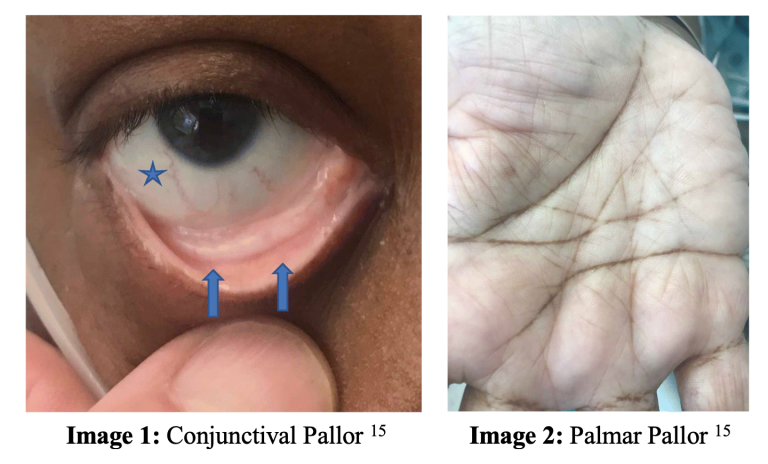
A 3-year-old male with G6PD deficiency presents to your ED by ambulance with shortness of breath, found to be hypoxic with SpO2 80% on 15L NRBM. He appears pale and dyspneic. The child is placed on HFNC with no improvement in saturation.
His remaining vital signs include T 36.6℃, BP 95/55, HR 160, RR 24.
Given his persistent hypoxia on noninvasive methods, a decision is made to intubate. Bedside CXR is unremarkable, and in spite of full ventilatory support with FiO2 of 100%, the patient’s saturation remains at 85%. You later learn he had eaten a full box of blueberries earlier that day.
Tibial Spine Fractures

A 13-year-old patient presents to the Emergency Department after sustaining a twisting knee injury while playing soccer. There was a pop, and the patient was subsequently unable to bear weight due to pain and knee instability. The swelling and pain increased in the hours after the injury occurred. On examination, there is a large knee effusion and a positive Lachman test. You obtain imaging (Figure 1). What is your suspected diagnosis? What is your initial workup in the ED? What imaging confirms the diagnosis? What is your management and disposition?
Are you sure you wish to end this session?

