Revision Resources
Recent Posts View All
April 2019 FOAMed
Basilar Skull Fractures
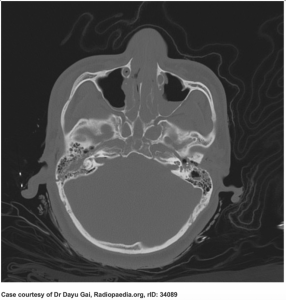
A 19-year-old male is brought to the ED by EMS status post MVC with a C-collar in place. The patient was restrained, there was no intrusion, and airbags deployed with the car traveling at 50 mph. Another passenger reports that the patient hit his head on the seat in front of him.
Triage vital signs (VS): BP 105/60, HR 88, T 99.2, RR 11, SpO2 94% on room air, GCS 12. Pertinent physical examination reveals hemotympanum, serosanguineous discharge bilaterally from the nares, and CN III palsy.
What’s the next step in your evaluation and treatment?
High degree AV blocks

The team at Medmastery are providing LITFL readers with a series of FOAMed courses from across their website. Over the next few weeks, we’ll be posting videos from the ECG Mastery: Yellow Belt and Blue Belt courses.
In this video, we look at high degree AV blocks on the ECG; the types of blocks and their clinical implications.
ED Management of Sickle Cell Vaso-occlusive Crises: Myths, Facts, and A Novel Approach to Acute Pain Management
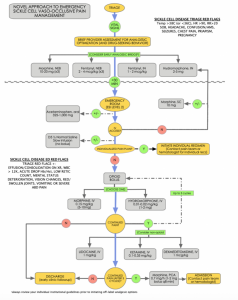
A 22-year-old male with known sickle cell disease presents to the emergency triage requesting opioids for what he feels is a sickle cell vaso-occlusive crisis. The patient indicates he missed his pain clinic appointment and has run out of his home Percocet prescription three days ago. Since then he has noted progressively worsening pain in his lower back and lower extremities that he believes was precipitated by an upper respiratory infection. He Indicates the pain is currently 10/10. He denies fever, chest pain, shortness of breath, vision changes, headache, or abdominal pain. The nursing staff is suspicious of drug-seeking activity as this is the third time in six weeks the patient has presented with similar complaints, each time specifically requesting ‘Dilaudid’.
The Critically Ill Infant
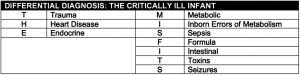
The critically ill infant is thankfully a rare event. Limited clinical exposure to these patients heightens anxiety and limits the development of a structured approach to their care. The goal is to develop a checklist for both supportive care and specific interventions than can make a difference in the first hour of care. Focus on the disease processes that are readily identifiable in the ED and are associated with successful interventions.
Guideline Review: ACEP 2018 – ED Procedural Sedation with Propofol

The last American College of Emergency Physicians (ACEP) guideline recommendations regarding the use of propofol for ED procedural sedation was in 2007. Much research has since demonstrated its safety in adults and children. Furthermore, many clinicians are co-administering ketamine or fentanyl in conjunction. This 2018 ACEP update addresses these issues and much more. The following infographic summarizes the key points.
Are you sure you wish to end this session?

