Revision Resources
Recent Posts View All
September FOAMed
RECOVERY-RS

Clinical Question – In hospitalised patients with COVID-19 requiring >40% FiO2 to achieve SaO2>94%, does the use of continuous positive airway pressure (CPAP) or high flow nasal oxygen (HFNO) compared with conventional O2 therapy (COT) reduce the incidence of tracheal intubation or death within 30 days?
Splenic Infarction: ED Presentation, Evaluation, and Management
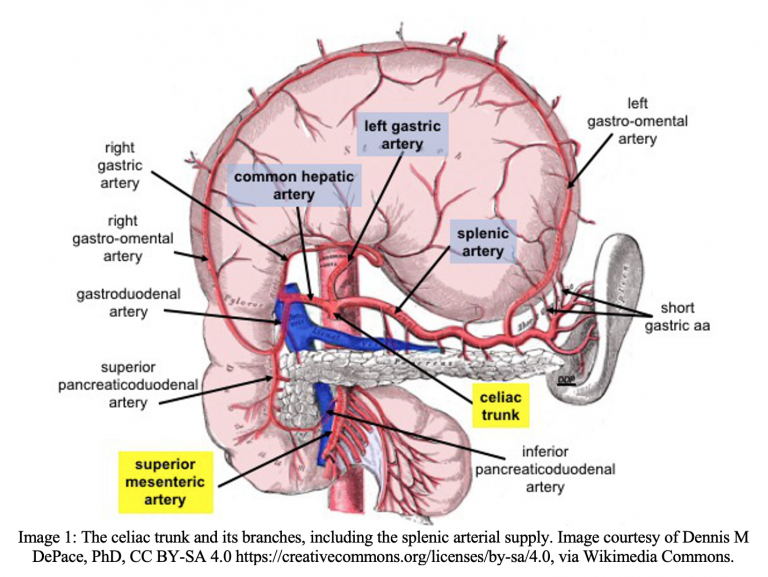
A 50-year-old male with a history of rate-controlled atrial fibrillation (non-compliant with warfarin), obesity, coronary artery disease, heroin use disorder, and hypertension presents with left-sided abdominal pain. He reports two days of worsening left flank and abdominal pain, chills, nausea, and two episodes of non-bilious, non-bloody vomiting this morning. He reports no significant changes in his diet or bowel movements. He denies trauma to the area or a history of abdominal surgeries. T 38.4C, HR 110, BP 155/95, RR 18, SpO2 99% on room air. On physical exam, his abdomen is soft and tender to palpation in the left upper-quadrant (LUQ) and left flank without rebound or guarding. Bowel sounds are within normal limits. No obvious masses or organomegaly are palpated, but exam is difficult due to body habitus. Labs show a WBC of 16 and LDH twice the normal limit. INR is 1.5. Bedside ultrasound of the LUQ shows no free fluid or subcapsular splenic hematoma. CT scan shows a wedge-shaped infarct in the upper pole of the spleen.
How High-Risk is a High-Risk BRUE?

Spoon Feed
Presence of AAP high-risk BRUE criteria do not accurately predict the presence of a serious underlying diagnosis. Abnormal medical history, history of similar event, event duration >1 minute, and altered responsiveness increased the odds of a serious underlying diagnosis.
Why does this matter?
The absence of high-risk criteria is an effective risk stratification tool to reduce unnecessary workup and admission in BRUE. However, does the presence of these criteria predict outcomes that warrant more than education and discharge, and if not, what does?
Crushing Chest pain, Tachycardia, and Very Elevated Blood Pressure in a 40-something Man.

A 40-something male called 911 for 2 hours of crushing, non-radiating, chest pain at about 11 AM. He reported a similar episode last year when his blood pressure was very out of control and that again he has not taken his BP meds for 2 months. He stated he had drunk 12 cans of Mountain Dew (high caffeine content) overnight.
On exam, he was very anxious, holding his chest, breathing normally. Chest pain was worse with palpation.
His BP was 250/150 with a heart rate of 150.
Necrotizing Fasciitis

The patient is a female in her 50s who presents following an injury to her right ankle approximately one week prior. The patient was fishing for catfish, and the barb from one of the catfish caused a puncture wound in her right lower extremity. She reports worsening erythema, edema, and pain in this area since the injury. She initially presented to an outside hospital three days prior and was sent home on oral clindamycin. She returned to the outside hospital again on the day of presentation due to worsening pain and malaise, and was found to be hypotensive, tachycardic, and hypoxic. She received intravenous (IV) fluids and cefepime and was transferred to our tertiary care medical center. On arrival, the patient remains alert and oriented but is tachycardic and hypotensive, so she is triaged to the shock resuscitation unit for further management.
Are you sure you wish to end this session?

