Revision Resources
Recent Posts View All
September 2018 FOAMed
PEM Playbook – The Pediatric Surgical Abdomen
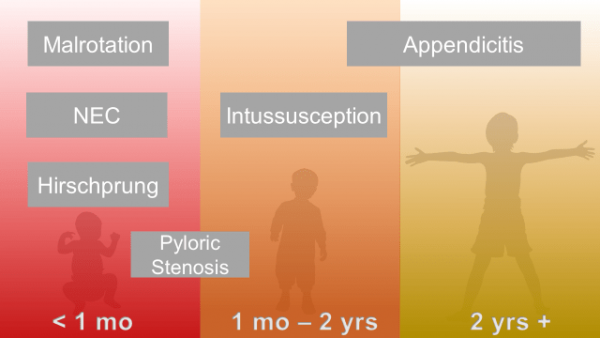
Abdominal pain is common; so are strongly held myths and legends about what is concerning, and what is not.
One of our largest responsibilities in the Emergency Department is sorting out benign from surgical or medical causes of abdominal pain. Morbidity and mortality varies by age and condition.
ECG Pointers: LVH vs STEMI

Only 15 minutes left of your busy overnight shift. You’re wrapping up your last chart when your attending looks at you and says, “The patient they just pulled back doesn’t look so good. You better go take a look…” You walk in the room and see an older African American male clutching his chest. He is diaphoretic and looks very uncomfortable. Your nurse hands you this EKG.
Cervical Spine Evaluation and Clearance in the Intoxicated Patient
Background: Alcohol and drug intoxication is common in trauma patients and a significant proportion of cervical spine (c-spine) injuries occur in patients with intoxication. A standard approach to both intoxicated and sober patients with suspected c-spine injury in many trauma centers includes the placement of a rigid cervical collar for spinal immobilization until the c-spine can be “cleared.” Even after a negative CT, intoxicated patients often are immobilized for prolonged periods of time until a reliable exam can be performed due to concern for missed findings on CT scan, specifically unstable ligamentous injuries. This practice is less than ideal, as prolonged c-spine immobilization is associated with DVT, atelectasis, aspiration pneumonia, and elevated intracranial pressures.
Common Psychiatric Medications: Pearls & Pitfalls for the ED
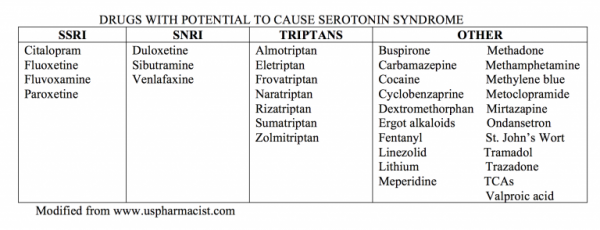
Emergency physicians encounter psychiatric medications in a variety of ways on any given shift. The acutely agitated patient who does not respond to verbal de-escalation may be chemically sedated, frequently with antipsychotics or benzodiazepines. Another, more common occurrence, is encountering a patient with a psychiatric history or one who is prescribed a drug for their emotional and/or mental health. Whether these drugs are listed in your patient’s medication list or a patient comes with an acute adverse reaction or overdose, it is critical to be familiar with several common psychiatric medications.
Focused Echocardiographic Evaluation in Life Support and Peri-Resuscitation (FEEL Study)
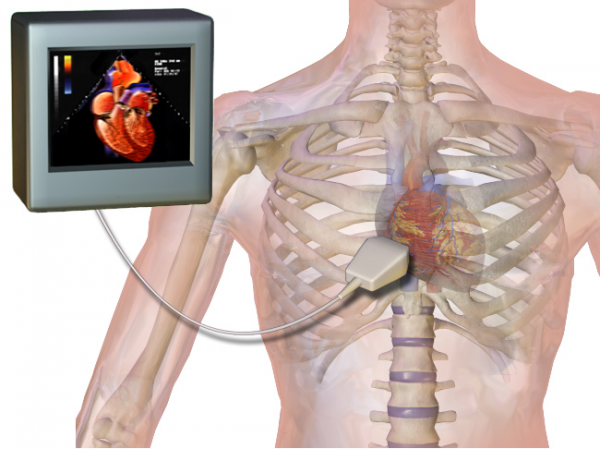
Focused use of ultrasound in resuscitation of patients with shock and cardiac arrest has become increasingly embraced in both the emergency department (ED) as well as in the prehospital setting. Application of ultrasound, particularly of echocardiography, has the potential to identify treatable causes of shock and arrest, identify shockable rhythms and identify the presence of mechanical activity. All of these can affect management decisions and, potentially effect outcomes. Recent studies have led to concerns that integration of point of care ultrasound (POCUS) in cardiac arrest increases pauses in compressions. Thus, it is important to establish what POCUS adds to shock and arrest management.
Are you sure you wish to end this session?

