Revision Resources
Recent Posts View All
November FOAMed
Postpartum Hypertensive Emergencies
In this 14-minute presentation from Rebellion in EM 2021, Dr. Jenny Beck-Esmay, MD discusses postpartum emergencies including hypertension, preeclampsia/eclampsia and HELLP syndrome. All of these entities frequently present through the emergency department, and failure to recognize these disease processes can lead to significant morbidity and mortality. This course will review the ED presentation and management of these disease processes.
Pneumothorax
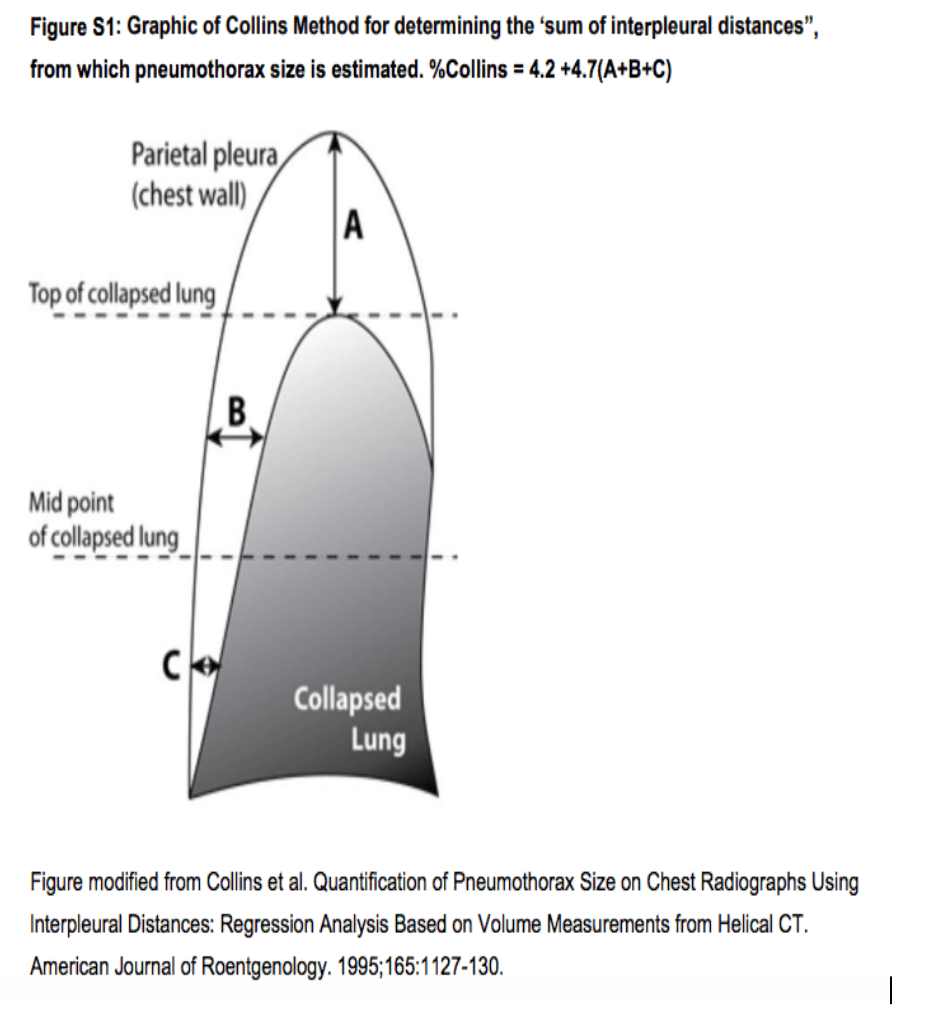
A quick overview of pneumothorax for the EM physician: the what, why, diagnosis, and treatment.
Alcohol binge and chest pain
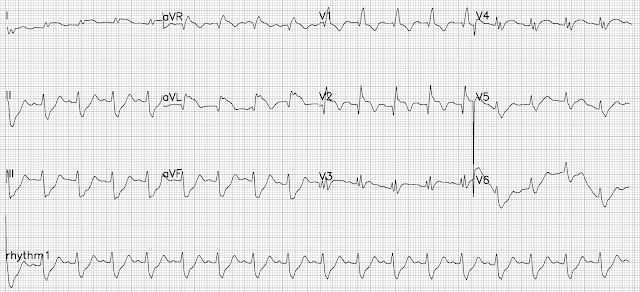
A man in his 30s was rushed into our ED on a Sunday morning with continuous chest pain for 2 hours. The patient was drowsy but following simple commands and was pointing to his left chest where it hurt with a single finger. He said the pain started after he tried to vomit forcefully. He also had the odor of alcohol to his breath. The patient voluntarily told the team he had half a bottle of whiskey the previous night and he was uncomfortable ever since he woke up. He did, however, consume alcohol on a regular basis but never at such high amounts.
Pediatric Abdominal Surgical Emergencies
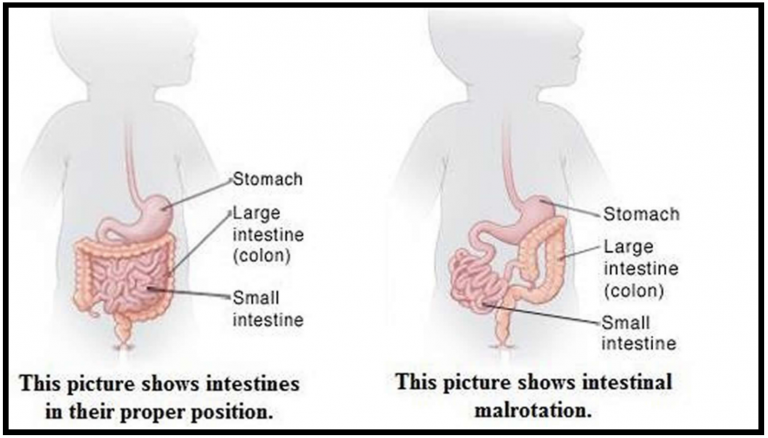
A 15-month-old male with no reported past medical history presents to the pediatric emergency department (PED) with fussiness of 2-day duration. The patient has intermittent episodes of fussiness during the past two day, during which he pulls his knees up to his chest. Initially, these episodes lasted for a few minutes at a time, and the patient was otherwise playful and interactive. As the days progressed though, he became more lethargic, has not been tolerating PO, and has had decreased wet diapers as per baseline. The mother also reports that the patient has had multiple episodes of non-bloody, non-bilious emesis over the past two days. She denies any fever, diarrhea, bloody stools, respiratory distress, recent travel or sick contacts. The patient is up-to-date with his vaccinations.
Calculation of the HEART Score
Not a single clinical shift passes without evaluation of at least one patient with chest pain. This chief complaint accounts for 6.5 million visits per year and is the second most common presenting symptom to the emergency department (ED). Additionally, there is substantial liability associated with missed coronary artery disease, accounting for the highest proportion of paid claims, 10.4%. This combination has led to a progression of lower incidence of true disease in patients admitted to the hospital for acute coronary syndrome, especially in those with two negative biomarkers (0.18%).
One of the tools that has emerged to assist ED clinicians in risk stratification of these patients is the HEART score. This tool was created to risk stratify patients presenting to the emergency department with chest pain for major adverse cardiac events (MACE) at 30 days (a composite of acute myocardial infarction, percutaneous coronary intervention, coronary artery bypass graft, and death). The tool incorporates both subjective and objective criteria.
Are you sure you wish to end this session?

