Revision Resources
Recent Posts View All
May FOAMed
Optimal Needle Position for Decompression of Tension PTX
Tension Pneumothorax (TP) can occur as a potentially life-threatening complication of chest trauma. With the risk of respiratory and cardiac arrest, an immediate temporizing intervention for this condition is required by direct Needle Decompression (ND). In 2018, the Advanced Trauma Life Support (ATLS) recommendations changed from the 2nd intercostal space in the midclavicular line (ICS2-MCL) to the 4th/5th intercostal space just anterior to the anterior-axillary line (ICS4/5-AAL), whereas the European Trauma Course (ETC) trauma guidelines and the guidelines from the Royal College of Surgeons of Edinburgh (RCSEd) in the UK still adhere to placement in the ICS2-MCL for the preferred location of ND. Both chest wall thickness of the patient and needle length both play a role in the success rate of ND. Although it is well known that Chest Wall Thickness (CWT) increases with BMI, it is unknown if the optimal place for ND may vary with BMI.
Anticholinergic Intoxication

Anticholinergic intoxication has been a moving target recently, with a resurgence in the popularity of physostigmine. The thoughtful administration of physostigmine has much to offer these patients, but it must be provided within the context of a systematic approach.
Lateral Canthotomy and Cantholysis

A 25-year-old male without any reported medical history presents to the emergency department with eye pain. He reports that 2 hours prior to arrival he was at his cousin’s house for Thanksgiving and per family tradition, there was a make-shift octagon in the back-yard for some friendly sparring. Despite the face being off-limits, one strike from his brother landed on his right eye. Since then he has had progressive pain and blurring of his vision in that eye. On initial examination, the eye is noted to be proptotic, and he is unable to move it in any of the cardinal directions. His vision is limited to only identifying light vs darkness. There are no obvious signs of globe rupture on initial assessment. Using an intra-ocular pressure meter you measure the intra-ocular pressure on the right to be 52 mm Hg. Given this initial presentation, you are concerned for a retrobulbar hematoma resulting in orbital compartment syndrome. What are your next steps? Is this a procedure you are planning to call in a subspecialist for? What if they are unavailable for emergent intervention?
Wound Care – Foreign Bodies

Take Home Points
- FBs are a very common complication of wounds.
- X-ray is poor at detecting foreign bodies
- US is a tremendous tool and be used dynamically at the bedside to assist w FB extraction
- Prophylactic antibiotics are not routinely recommended
Cervical Vessel Dissection
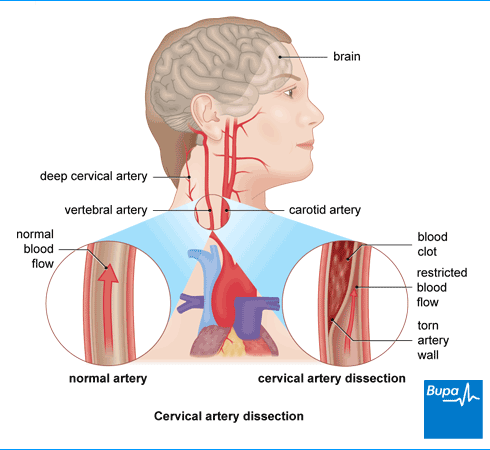
Case 1:
A 32-year-old male presents with headache and neck pain. This is his second visit in the last week. 10 days ago he was in a motor vehicle accident and had a negative non contrast head CT and C spine CT at that time.
Case 2:
A 38-year-old female presents with anterior neck pain. You notice ptosis and miosis on exam, but no anhydrosis.
Case 3:
A 31-year-old female presents with focal motor weakness in the left arm and leg. Her husband states she was complaining of a headache and neck pain several days ago. A “Code Stroke” is activated.
Are you sure you wish to end this session?

