Revision Resources
Recent Posts View All
March FOAMed
Emergency Contraception For Teenagers
Olivia presents to the children’s emergency department at 3:40 one Monday afternoon still in her school uniform and with her friend Annabel. Annabel does all the talking to start with and tells the receptionist her friend has “a gynae problem”. She is somewhat assertive with the triage nurse arguing that Olivia needs to be seen by a doctor, in a private room and not in a cubicle with curtains. They disclose that they are both 15 years old. When you arrive in the room, Olivia tells you she’s come to A&E to get “the morning after pill”.
Spinal Epidural Abscess
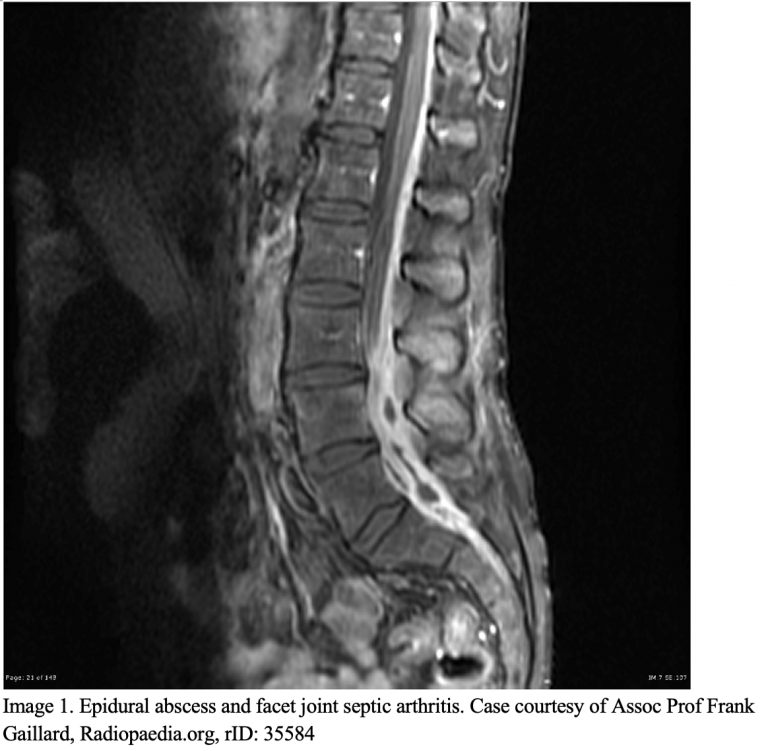
A 48-year-old woman presents to the ED with a ten-day history of low back pain that she notes began after lifting boxes in her garage. She has a past history of injection drug use and rheumatoid arthritis controlled with methotrexate. She sought care two days earlier at an urgent care and was prescribed cyclobenzaprine for a presumed lumbar sprain. She has had intermittent fevers that improve with acetaminophen, but her pain has grown worse in the past 72 hours, now occurring with shooting sensations down her legs bilaterally. On exam, her vitals are stable with a temperature of 99.4 ℉. She has mild weakness in her left lower extremity and full bilateral extremity pulses. What is the next step in evaluation?
The Inconsolable Infant

A 2-month-old male infant born by uncomplicated spontaneous vaginal delivery at 38 weeks presented with two days of crying and irritability. Mom stated the baby’s birth was normal and he has been growing and developing normally. Two days ago, he became fussy, and has been crying and inconsolable since. He has been feeding well and making normal wet diapers. A thorough review of systems identified no other associated signs or symptoms. The patient’s vital signs were normal. Physical exam was notable for a fussy but well-appearing baby boy. Mucous membranes were moist. Fontanelle was flat. Heart sounds were normal without murmurs. Pulses were full on all extremities. Abdominal exam was reassuring with no hepatosplenomegaly, no guarding, no masses and no obvious ecchymosis. He had normal suck and moro reflexes. His tone was good. A thorough skin exam revealed no abnormalities. There were no outward signs of trauma.
Benign Paroxysmal Positional Vertigo
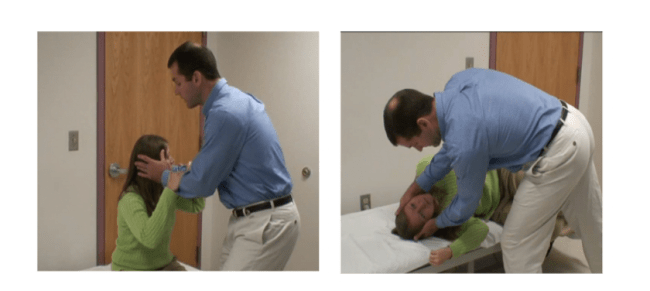
A 63-year old female presents to your ED with positional dizziness since rising out of bed from a nap this afternoon. She says she had a similar episode in the past and reports, “they took the stones out of my ear by making me lay down and move my head a few times.” Based on your assessment of the patient’s history and physical exam you determine she has peripheral vertigo, likely BPPV. However, despite multiple attempts with the Epley Maneuver, the patient is still symptomatic. What next steps could you consider?
Tympanic Membrane Rupture
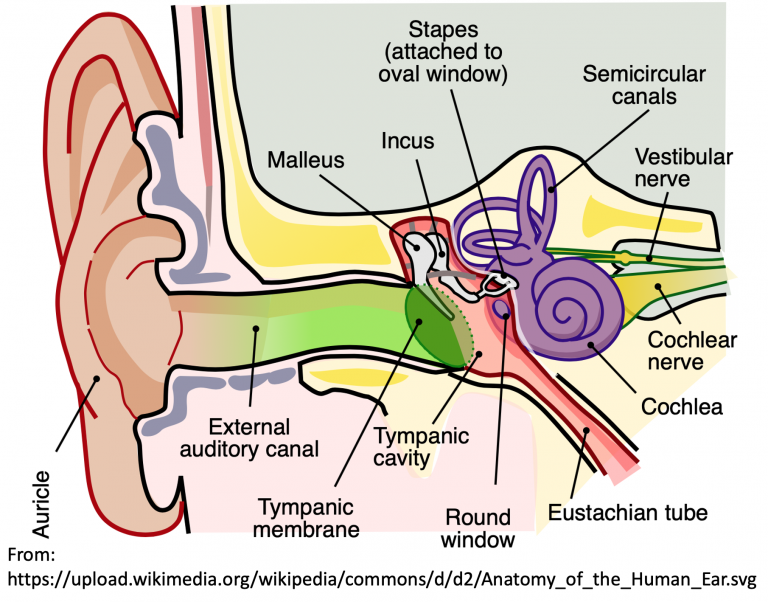
A 31-year-old female presents with right ear pain and decreased hearing. Her symptoms started suddenly after trying to clean her ears with a Q-tip. She denies vertigo, nausea, vomiting, or other facial symptoms. She has no past medical/surgical history and has no allergies. On examination, her vital signs are normal. You see a small perforation in the tympanic membrane (TM) with no discharge or other trauma. What is your next step in evaluation and management?
Are you sure you wish to end this session?

