Revision Resources
Recent Posts View All
January FOAMed
Myocarditis

A 24 y.o.female with past medical history of C-section (2 years ago) presented to the ED of an OSH complaining of chest pain. Patient was in her normal state of health recently until 3 days ago when she began having intermittent, diffuse, midsternal, non-radiating chest pain associated with shortness of breath and subjective fevers. Pain is aggravated by nothing but relieved somewhat by leaning forward. Patient also states she had some nausea and NBNB vomiting of approximately 5 episodes during the last 3 days and after the first episode of vomiting she also began to have intermittent non-radiating epigastric pain. Denies diarrhea, urinary complaints, or any recent abdominal or chest trauma. Of note patient states she was tested positive for COVID-19 in April 2020 (6 months ago). She was not hospitalized and recovered without incident per patient report.
Systematic Approach to the Peripheral Vascular Exam

A 62-year-old male with a history of hypertension, congestive heart failure, type II diabetes mellitus, and tobacco use presents to the emergency department (ED) with severe left lower leg pain that started six hours ago. Notably, he works as a long-distance trucker. Vital signs are notable for tachycardia to 116 bpm and a blood pressure of 160/89 mmHg. Upon further questioning, he notes that he was diagnosed with peripheral arterial disease (PAD) a few years ago, but that pain is only present with ambulation. His current pain is worse and present at rest.
A Regular to the ED

A 45-year-old male with no fixed address is found by a bystander with decreased level of consciousness (LOC) on the street. Emergency Medical Services (EMS) is called, and the patient is brought to the emergency department (ED). An empty bottle of vodka is found on the patient, and the decreased LOC is suspected to be due to alcohol intoxication. It is the patient’s fifth visit to the ED in the last two weeks with a similar presentation. The patient is observed over many hours, their LOC improves, and they are discharged after demonstrating that they can ambulate safely.
Acute Mitral Regurgitation
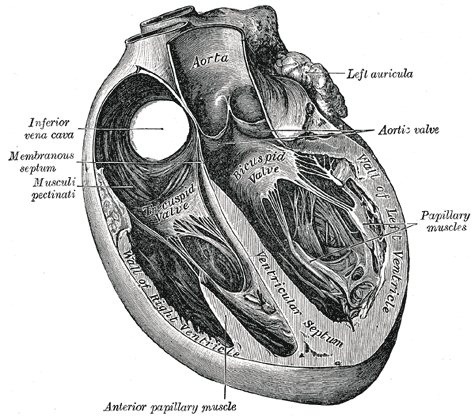
The patient is a 52 year-old female with a past medical history of hypertension, hyperlipidemia, hypothyroidism, and a 2 pack a day smoking history who presented to the emergency department in respiratory distress. When EMS arrived to the patient’s home, she was hypoxemic with a pulse oximetry reading of 70s on room air and hypotensive with systolic blood pressures in the 80s. She was placed on nasal cannula with improvement in her saturations and she was given aspirin, fentanyl, and nitroglycerin without relief. Upon arrival her vitals were significant for respiratory rate of 34, pulse oximetry of 98% on 6L NC. She was noted to be in acute distress.
Necrotizing Pancreatitis
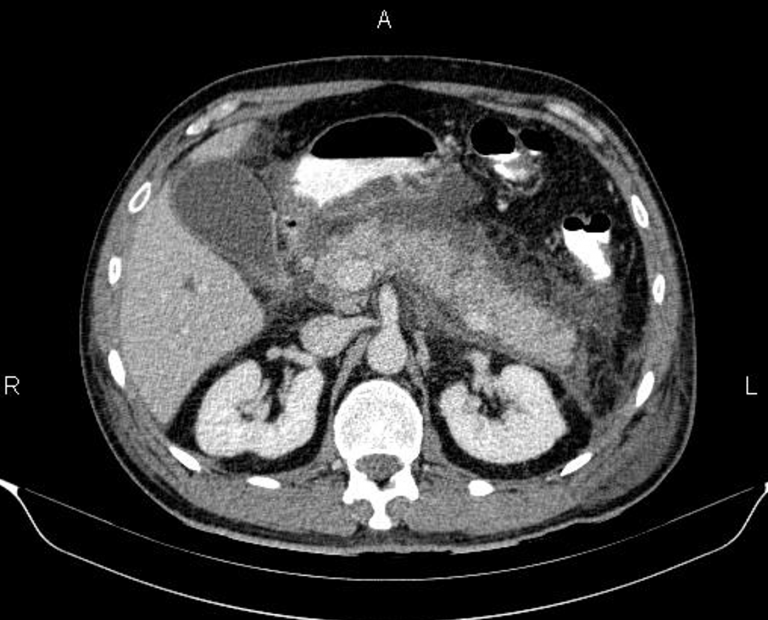
A 40 year-old patient presents with increasing abdominal pain and a new fever. She initially presented to the Emergency Department five days prior for upper abdominal pain. The initial workup showed stable vital signs, mildly elevated lipase, and an unremarkable right upper quadrant ultrasound. The patient was diagnosed with gastroenteritis and discharged home with primary care follow up. She now returns to the Emergency Department five days later with increased abdominal pain and feeling overall unwell.
Are you sure you wish to end this session?

