Revision Resources
Recent Posts View All
December FOAMed
Right Heart Failure in the ED
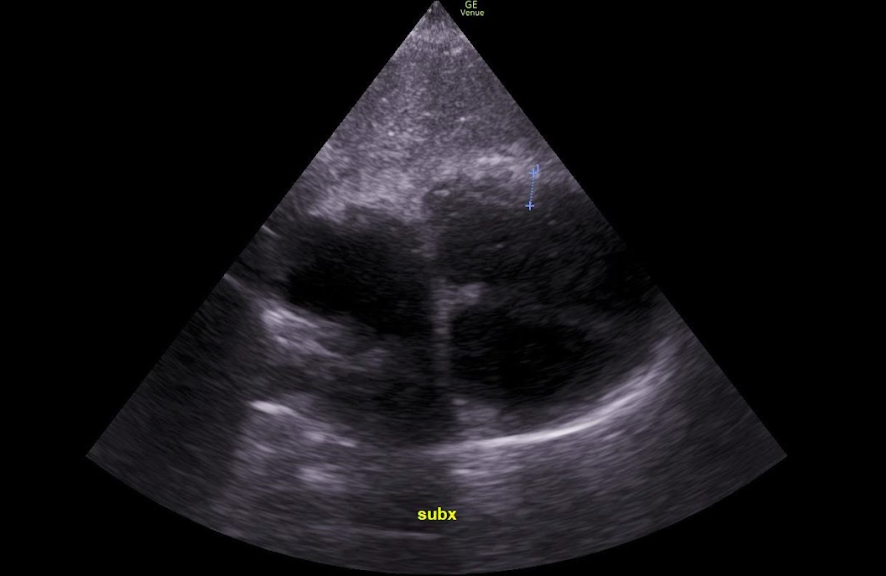
A 58-year-old male with a history of CAD, HTN, and a 40-pack-year smoking history presents to the emergency department (ED) for shortness of breath (SOB). His SOB has been progressive for one week but has acutely worsened over the last day. The patient has associated chest tightness, wheezing, and worsening of chronic leg swelling. He was treated two months ago for bronchitis. HE tried using some nebulized albuterol at home but his symptoms persisted, prompting the ED visit. The patient is vaccinated against COVID and he was infected with COVID one year ago. Vital signs on arrival to the ED are HR 120 bpm, BP 76/42 mm Hg, RR 30 per minute, O2 87% on room air, T 37.0 C (98.6F). On exam, he has moderate respiratory distress with diminished breath sounds bilaterally and bilateral pitting edema to the lower extremities. ECG is negative for STEMI and a stat portable CXR is negative for pneumonia, pneumothorax, or pulmonary edema. While the differential diagnosis in this patient is broad, careful consideration in the next steps of resuscitation and management in order to “do no harm” is necessary.
Didtended Abdomens in Neonates

Abdominal distention is common in neonates. The challenge is differentiating pathological causes of abdominal distension from benign ones. But first, we need to consider what, exactly, defines a distended abdomen.
Infectious Mononucleosis

A 17-year-old male with history of asthma presents to the ED with a chief complaint of sore throat for the past 3 days, associated with decreased oral intake. He denies sick contacts. Vital signs include Temp 100.6F, BP 124/78, HR 92, RR 16, 96% on RA. On exam the patient has swollen, erythematous tonsils with grayish exudate, as well as enlarged, tender anterior and posterior cervical chain lymph nodes.
Post-Cardiac Arrest Hypotension

During a cardiac arrest resuscitation, finally palpating a pulsatile flow beneath your gloved fingertips brings a sense of satisfaction like no other. But just as you go to finally breathe a sigh of relief and wipe the beading sweat off your brow, your now widening pupils focus on the patient’s steadily plummeting blood pressure. As you begin to sense your own heart palpitating, you think about medications to utilize in hopes of staving off another round of chest compressions. Since you’ve already given four doses of code-dose epinephrine, maybe an epinephrine infusion is best? You also recall that norepinephrine seems to be a popular choice in patients with shock, so maybe you should start that instead?
Methemoglobinemia
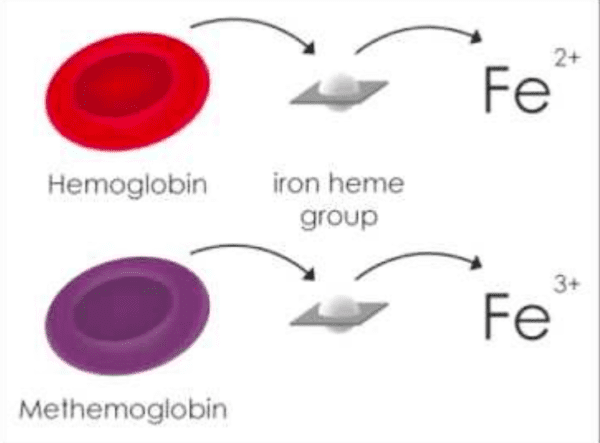
Methemoglobinemia can result from exposure to a number of different medications. The most common are dapsone and topical anesthetic agents (i.e. benzocaine)
Consider the diagnosis in any patient with cyanosis and hypoxia that doesn’t respond to oxygen administration
Administer methylene blue to any patient with abnormal vital signs, metabolic acidosis, end organ dysfunction or, a serum level > 25%
Are you sure you wish to end this session?

