Revision Resources
Recent Posts View All
August FOAMed
Sciatica Mimics

A 64-year-old male with a past medical history of hypertension presents to the emergency department with right lower back pain. He states the pain started when he bent down to reach for dishwasher detergent yesterday evening. He feels the pain starting in his lower back and radiating down the leg. He denies any recent trauma or similar symptoms in the past. He denies bowel or bladder incontinence, weakness, sensation changes, fevers, or recent weight loss. You suspect his presentation is consistent with sciatica. How is sciatica diagnosed and what are some mimics that comprise the differential diagnosis?
Bronchopulmonary Dysplasia
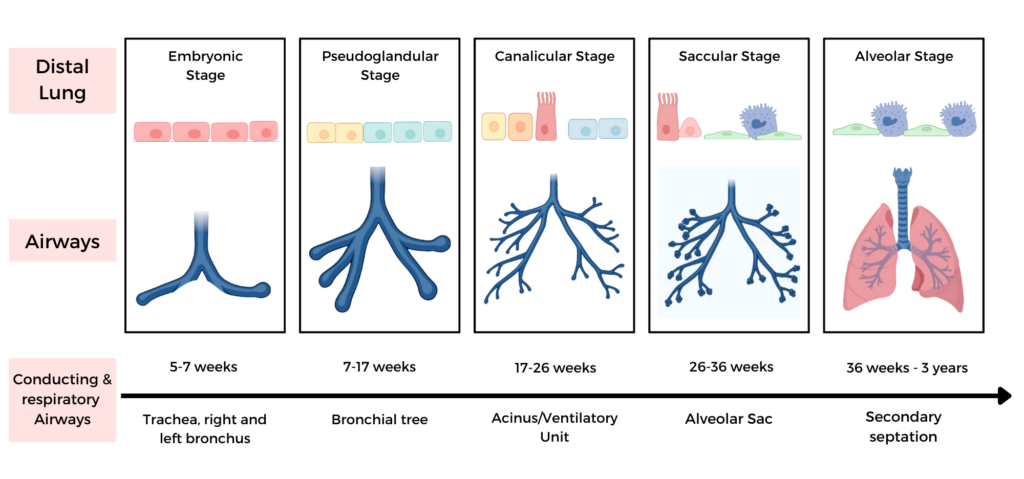
Jess is an ex-26 plus 4 weeker, born via spontaneous vaginal delivery. No antenatal corticosteroids were given. She was relatively well at birth and was admitted on CPAP to the NICU. She developed respiratory distress two hours after birth. She was promptly intubated and surfactant administered. She is currently 37 weeks corrected gestational age and is still on high flow nasal cannula oxygen. Her parents are concerned about the long-term consequences of her chronic lung disease.
Neuromuscular Disease

There is a long list of rare neuromuscular diseases. Nonetheless, there are a few that you are likely to see in the ED, that are relevant to Emergency Medicine because they require timely diagnosis and treatment. In this Part 2 of our 2-part series on acute motor weakness with Roy Baskind and George Porfiris, we keep it short and simple by limiting our discussion to the key clinical clues and management strategies of two of the more common acute life-threatening neuromuscular diseases, myasthenia gravis and Guillain Barré syndrome, and how to distinguish them from their mimics…
Sudden Hearing Loss - Guideline

I think this is a reasonably well done guideline. I am only providing a very basic summary here. For each recommendation, this guideline provides a brief discussion under each of these headings: “quality improvement opportunity”, “aggregate evidence quality”, “level of confidence in evidence”, “benefits”, “risks, harms, costs”, “benefit-harm assessment”, “value judgements”, “intentional vagueness”, “role of patient preferences”, “exceptions”, “policy level”, and “differences of opinion”. As a result, there is an easy to read summary that gives you a good sense of not just the recommendations, but the uncertainty and debate that underlies the recommendations.
Impaled Objects
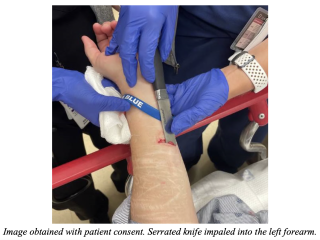
A 60-year-old female presents to the ED with an impaled object in her arm. She reports stabbing herself in the left arm as an act of self-harm, prior to calling EMS. She reports pain and scant bleeding from the injury site. She left the object in her arm due to fear that removing it would cause more injury. The object was wrapped in gauze by EMS, and she was transported to the ED. On initial assessment on arrival vital signs are BP 150/90, HR 86, RR18, SpO2 96% on RA. She is alert and oriented, talking in complete sentences, bilateral breath sounds are clear, and she has 2+ pulses in the upper extremities. Under extensive gauze wrapping, there is a large, serrated knife impaled in the distal aspect of the left flexor forearm. It is superficial and can be easily palpated along the skin. There are no other injuries identified on primary and secondary surveys. Her left arm as a 2+ radial pulse, along with brisk capillary refill, intact sensory and motor function to distal hand and fingers.
Are you sure you wish to end this session?

