Revision Resources
Recent Posts View All
April FOAMed
Bradycardia

Case 1:
A 75-year-old female presents 4 hours after ingesting several metoprolol doses accidentally. She feels lightheaded and slightly confused. HR is 42, with a blood pressure of 81/44.
Case 2:
A 43-year-old male with ESRD on hemodialysis presents after an episode of syncope. He feels short of breath and tired, but he denies other symptoms. He has missed two sessions of hemodialysis. His heart rate is 55, with a blood pressure of 122/73.
Eating Disorders

Eating disorders [ED] can have devastating effects on the lives of young people and their families. The patient journey is isolating and often characterised by a lack of insight into their frailty. Sadly, EDs can be under-recognised and undertreated, with many opportunities to intervene missed. The mnemonic CARE (Consider, Ask, Risk assess, Everyone) may aid the recognition and risk assessment whilst encouraging holistic support of young people with eating disorders, and their families.
Dead Space
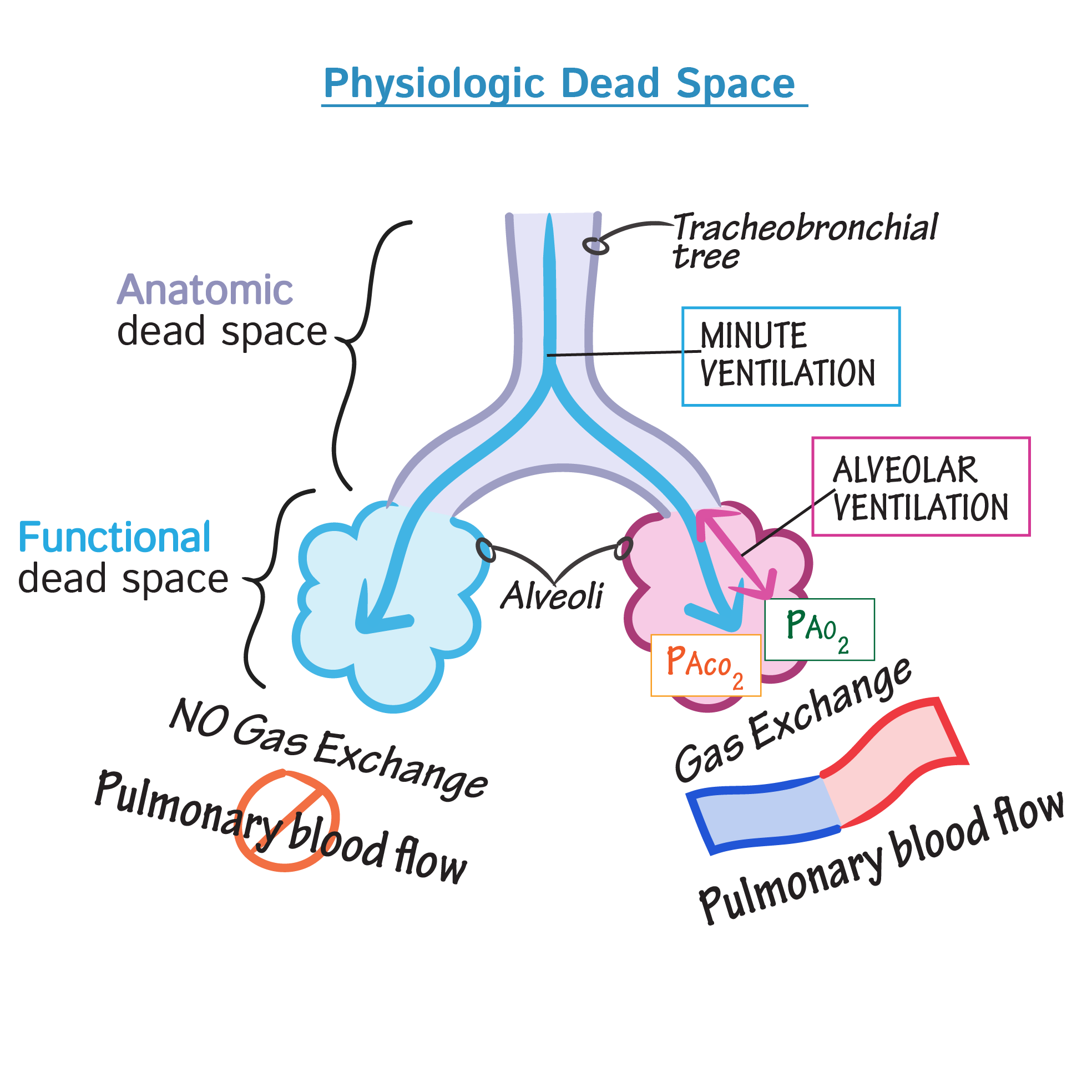
Today we’re talking about dead space. While it may sound like something from The Expanse, we’re actually talking about the physiological concept of dead space here. This is pretty core physiology that crops up in clinical practice all the time so I think it’s worth thinking about.
As usual this represents a sort of idiot’s guide to the topic with just enough information to scrape by in an exam and in clinical practice but likely with large gaps, simplifications and occasional frank errors in description.
Pericardial Effusion and Tamponade
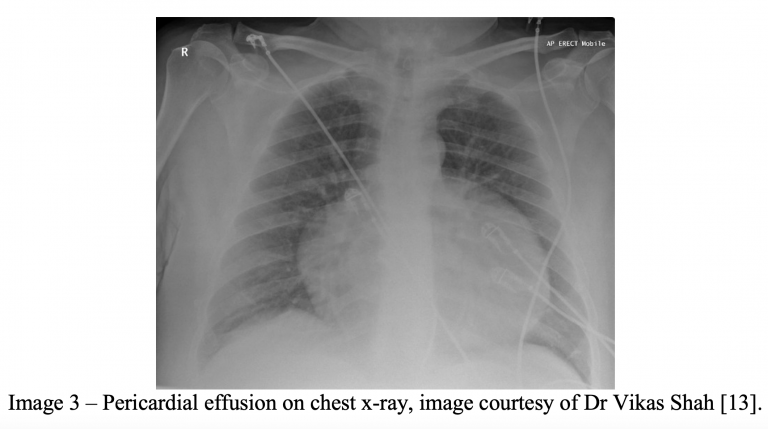
A 75-year-old male with a past medical history of hypertension, hyperlipidemia, and tobacco use presents to the emergency department with chest pain and shortness of breath. The patient describes his chest pain as a dull, pressure-like sensation that worsens with lying flat. The patient describes worsening dyspnea on exertion over the past 24 hours. The patient is placed on telemetry monitoring with pulse oximetry as intravenous lines are established. Vital signs include BP 92/50, HR 107, oxygen saturation 95% on 4L via nasal cannula. An electrocardiogram demonstrates sinus tachycardia with global low voltage and QRS complexes of varying amplitudes from beat-to-beat.
PPIs in GI Bleeds

The topic of PPIs for upper GI bleeds was one of the first posts on First10EM. There is no new evidence, and the bottom line is the same (just don’t use them), so if you are a long time reader, you can probably skip this post. However, that post was rather messy, and needed some updates. If you are still using PPIs, or know someone who is, this is the evidence summary for you.
Are you sure you wish to end this session?

