Revision Resources
Recent Posts View All
May 2018 FOAMed
The SIRS & qSOFA Confusion in Sepsis

It is well established that the rapid identification of patients with sepsis is needed in order to initiate timely care to improve morbidity and mortality. The systemic inflammatory response syndrome (SIRS) criteria have been used for some time for screening, however the sensitivity and specificity of these criteria have been brought to question based on recent evidence. This may have been one of the many reasons why the Sepsis-3 task force recommended the quick sequential (Sepsis-related) organ failure assessment (qSOFA) for prediction of mortality in sepsis. qSOFA consists of low blood pressure (SBP ≤100mmhg), increased respiratory rate (≥22bpm), and altered mental status (GCS ≤14). 2 or more of these criteria indicates an increased risk of death. There have been several studies calling into question the sensitivity of this criteria. In this post, we will review a recent systematic review and meta-analysis assessing the prognostic value of qSOFA vs SIRS in adult patients with suspected infection in the ED, hospital wards, and the ICU.
Complications of anticoagulation and how to manage them.
So, this was the lecture title I was given for the RCEM CPD conference this year for the geriatric medicine session. Quite the opposite of what I usually talk about, which is thrombosis and why we should anticoagulate everyone. Having said that there is no denying the link between bleeding and clotting. We set up our local thrombosis committee as a ‘thrombosis and anticoagulation committee’ for example, realising that it would be futile to try and tackle just one half of this issue. FOAM also gets this, evidenced by the recently launched ‘blood and clots’ series from Canada. As my friend and colleague Kerstin de Wit always says, ‘clotters bleed and bleeders clot’. How we manage the 2 competing pathologies is sometimes very tricky.
Hyperglycemic Hyperosmolar Syndrome

An acute decompensated state in which patients manifest a change in mental status in the setting of hyperglycemia, hyperosmolarity and severe volume depletion. Altered mental status can present as focal neurologic defects or global encephalopathy.
Power and Sample Size
In this Editorial, Professor Imelda Galvin from Queen’s University in Canada takes us through the details of Power, how it relates to trial sample size, and why it matters.
Esophageal Perforation: Pearls and Pitfalls for the Resuscitation Room
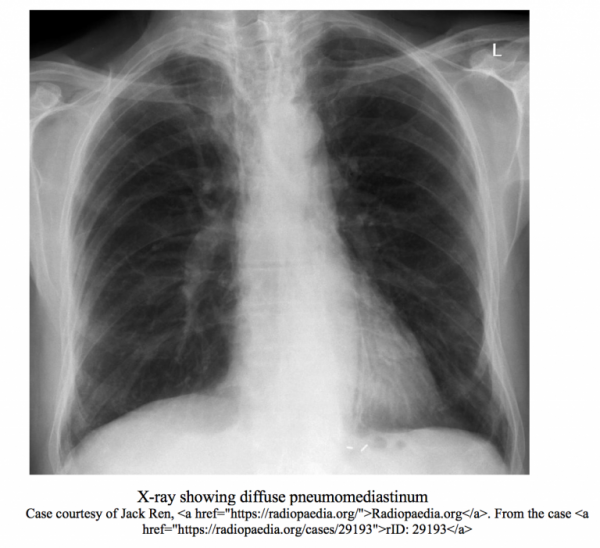
A 22 y/o female presents to the ED via EMS for several hours of progressively worsening chest pain and shortness of breath. As per EMS, patient was in respiratory distress on scene, with poor air entry in the setting of a history of asthma and was given multiple albuterol nebulizer treatments, solumedrol 125mg IV, and magnesium 2gm IV with minimal improvement. She is brought immediately to the resuscitation room, IV access is confirmed, and is placed on a cardiac monitor while receiving continuous nebulizer treatments via non-rebreather mask. Initial history is limited due to dyspnea. The mother of the patient also arrived with EMS and affirms the patient has a history of asthma, depression, and body dysmorphic disorder and has been dieting heavily over the past several weeks.
Are you sure you wish to end this session?

