Revision Resources
Recent Posts View All
January 2018 FOAMed
Reversing NOACs – Updates for Emergency Physicians
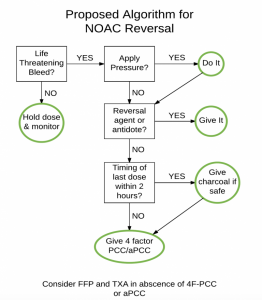
An 80-year-old female is brought to your institution unresponsive after she fell and hit her head. She has a history of nonvalvular atrial fibrillation. Her family is unsure of the exact agent, but knows that she is on a newer anticoagulant. Prior to this event the patient has lived a very active, independent, and vibrant life. You perform standard ATLS stabilization, and ultimately the patient is diagnosed with a subdural hematoma. How will you reverse her if her anticoagulant is dabigatran? Apixaban?
How to ask a question at a conference. The origin of ‘that’ algorithm.

To get you started we need to tell you a bit of a story. Sit back, relax, and remember a conference you’ve recently attended. Remember the feel of the seat and the hall. Imagine you’re back at the conference and a speaker has just given a reasonably interesting talk on something relevant to your speciality. You’ve listened and learned a few new things, heard a couple of surprising facts that you’re going to go away and think about. You’re just pulling out the conference program to see what’s up next and then the moment happens. The session chair invites questions…….
MARSIPAN – Not just for (Christmas) Cakes.
A few weeks ago I did a straw poll of EM doctors – I asked, ‘If I said MARSIPAN Guidelines to you would you know what I was talking about? There were several answers about Christmas cakes, but otherwise the answer was ‘No’.
It didn’t surprise me that much, I probably wouldn’t have known myself a couple of years ago, but as they relate to the psychiatric illness with the highest mortality of all. Stop for a moment and think what that diagnosis could be? Hold that thought and then just agree with me that if we have a disease with a really high mortality that can present to the ED then it’s our business to know how to recognise it and what to do about.
Hamman’s Syndrome and DKA – Ped EM Morsels

Certainly there are many issues to consider while diagnosing and managing diabetic ketoacidosis (DKA), like the possibility of cerebral edema. Often, these ill patients complain of significant nausea and abdominal / chest pain as well. Before we just attribute those symptoms completely to the pathologic process of DKA, let’s consider the potential complication of pneumomediastinum by being vigilant for Hamman’s Syndrome.
Acetaminophen or NSAID for Acute Minor Musculoskeletal Pain

Acute, minor musculoskeletal injuries (i.e. non-fracture or dislocations) are frequently seen in the Emergency Department. Aside from ruling out a more severe injury, management often focuses on pain relief or mitigation of pain. Though many analgesic agents exist, acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used for this indication. Both have important side effects or potential for adverse events that must be considered when prescribing them. Finally, it is unclear if combining the two classes of medications is beneficial.
Occult Knee Injuries Pearls and Pitfalls – EM Docs

There are a whole slew of very important occult knee injuries – those that have a normal or near normal x-ray – that can cause serious morbidity if you miss them, and for the catchall soft tissue injuries there are some subtleties in diagnosis and management that will make a real difference to our patients. When should we suspect a spontaneously reduced knee dislocation? Do all patients suspected of a spontaneous knee dislocation require a CT angiogram to rule out vascular injury? Which patients with a low energy mechanism are at risk for knee dislocation and vascular complications? How can you increase the accuracy of the active straight leg raise in assessing for quadriceps and patella tendon rupture? What is an easy way to identify patella baja and patella alta? What are the true indications for a knee immobilizer and how can knee immobilizers kill our patients? and many more…
Are you sure you wish to end this session?

